
YOUR BRAIN ON MENOPAUSE: In this seven-part series I explore menopause from a brain health perspective with a particular focus on the neurobiology of hot flashes, sleep, mood and memory, the role of hormone therapies and their long-term effects on the brain. This is Part 2.
This is a long and detailed read. Click here to download the series as a PDF to read offline.
The pattern of hormone changes across the entire menopause is very well characterised. But each woman follows her own hormonal trajectory. Like puberty and pregnancy (and all life experiences, really), there is huge variability between women, stages, stage length, types and severity of symptoms.
To understand how hormones and the brain chat, let’s turn the clock back to … puberty!
The HPO axis and the tick-tock of your biological clock
Popular wisdom would have you think puberty begins in the ovaries and a young body suddenly steeped in oestrogen grows curvaceous and fecund. Whilst puberty ‘proper’ involves the ovaries, the action really all kicks off up in the brain.
To understand the neurobiological underpinnings of puberty (and menopause), we need to understand the HPO axis, a trio that unites body and brain and orchestrates our reproductive lives.
In brief, the HPO axis works like this:
- Hypothalamus (H) signals to the Pituitary Gland (P) via the gonadotrophin-releasing hormone (GnRH).
- Gonadotrophic releasing hormone (GnRH) causes the release of luteinising hormone (LH) and follicle-stimulating hormone (FSH).
- LH and FSH stimulate the Ovaries (O) to release oestrogens and progesterone.
- Oestrogen and progesterone exert their wide-ranging effects on the body and brain.
- LH, FSH, oestrogen and progesterone signal back to the hypothalamus and pituitary forming complex positive and negative feedback loops of the H-P-O axis.
The complex positive and negative feedback loops of the HPO axis.
During our fertile years between puberty and menopause, GnRH is secreted from a pulse generator in the hypothalamus in a rhythmic fashion. I like to think of it as the neural manifestation of the famed biological clock – tick-tick-tick. This ensures the smooth and predictable production and coordination of all the other hormones in the loop.
The hormonal trajectory of menopause
During perimenopause, the HPO axis that has been conversing merrily since puberty starts to sputter. Thus, the phase of life is characterised by erratic and unpredictable ovarian hormone production. Our ovaries can still make oestrogen, but just not reliably and in the right quantity. As your ovaries wind down their duties and head toward retirement, the ovarian-brain conversation falters, then disconnects altogether.
The knock on effect is not, as you’d expect, flat-lining of all hormones…
- GnRH is produced by the hypothalamus and controls the synthesis and secretion of LH and FSH in the pituitary. Ovarian hormones influence GnRH secretion via feedback loops between the ovaries and brain. Since the onset of puberty, GnRH is released in a rhythmic tick-tick-tick. During early perimenopause, the GnRH beat slows to an erratic ‘tock…tick-tock ……… tock’.
- Luteinising hormone (LH) is produced by the pituitary gland, and, like its hypothalamic conductor is released in a pulsatile fashion. LH stimulates the ovaries to convert testosterone to oestradial, and during our fertile years, a mid-cycle surge of LH triggers ovulation. During menopause, LH levels remain normal initially before skyrocketing as they valiantly try to signal to the wearying ovaries.
- Follicle-stimulating hormone (FSH), also produced by the pituitary gland, stimulates the production of oestradiol and progesterone. Starting at the beginning of puberty, FSH is secreted in parallel with LH and the LH-to- FSH ratio is one-to-one. A subtle rise in the levels of FSH is the earliest and most consistent clinically measurable hormonal change. If you’re sent for a blood test to determine your menopausal status, the test will be for increased FSH levels. After menopause FSH levels shoot up.
- Oestrogen levels increase during puberty, fluctuate for a while, level off as ovulation is established, and barring pregnancy or the pill, cycle regularly each month till early perimenopause. Oestrogen levels become erratic and elevated throughout early perimenopause, then decrease and become less erratic towards the end of perimenopause. They finally bottom-out altogether post-menopause.
- Progesterone is manufactured by the corpus luteum after ovulation. Production ceases if the egg is not fertilised, upon which menstruation occurs. Girls and young women tend to have low or variable progesterone levels during the first few years after menarche. Progesterone decreases gradually but continuously during perimenopause.
And the two hormones relevant to menopause you may not have considered are ….
- Testosterone is produced in the ovaries and adrenal glands. Levels peak in our 20s and decline slowly but steadily until old age. Both ovaries and adrenal glands continue to make testosterone even after the testosterone to oestrogen conversion halts.
- Oestrone is a type of oestrogen. From puberty, about half our body’s oestrone is produced by the ovaries, and the other half by fat tissue and the adrenal glands. After menopause, oestrone is the predominant oestrogen, but has only 4% of the activity of estradiol, so its influence is really very weak. After menopause its production continues in fat tissue and is thought to play a role in modulating bone density.
Some brain areas are rich in oestrogen receptors
In general, hormones exert their effects on neurons and other cells by latching on to specific hormone recognition sites called receptors.
Hormones can only act on a cell when their receptor is present. Think of a lock and key where the receptor is the lock and the hormone is the key. Turning the key sets off a cascade of biological responses inside the cell.
Receptors for oestrogen are found throughout the brain. Mostly in areas associated with reproduction (e.g. the hypothalamus and pituitary), cognition (e.g. the cerebral cortex) and emotion (e.g. the hippocampus and amygdala). The widespread distribution of ovarian hormone receptors and actions on neurons indicates they have a wide-ranging effect on how we think, feel and behave.
Here’s a more detailed list of oestrogen-receptor rich brain regions.
- Preoptic nucleus of the hypothalamus — regulates temperature (has perhaps more oestrogen receptors than anywhere else in the brain).
- Suprachiasmatic nucleus (SCN) of the hypothalamus — regulates sleep and circadian (light-dark) rhythms.
- Hippocampus — learning and memory, emotion processing
- Amygdala — emotion and motivation
- Cingulate cortex — learning and memory, emotion processing
- Raphe nucleus — mood (serotonin hub)
- Locus coeruleus — attention, arousal and anxiety (noradrenaline hub)
- Prefrontal cortex — executive function and working memory
Adding another layer of complexity, oestrogen is locally synthesised in the brain.
Curiously, there are few human brain studies available for the distribution of progesterone receptors, so we assume from animal studies they’re found in broadly the same areas as oestrogen receptors.
Oestrogen may impact neuroplasticity
Oestrogen and progesterone alter the way in which neurons communicate with each other at the synapse, and affect all major neurotransmitter systems including those that use noradrenaline, dopamine, serotonin, glutamate and GABA.
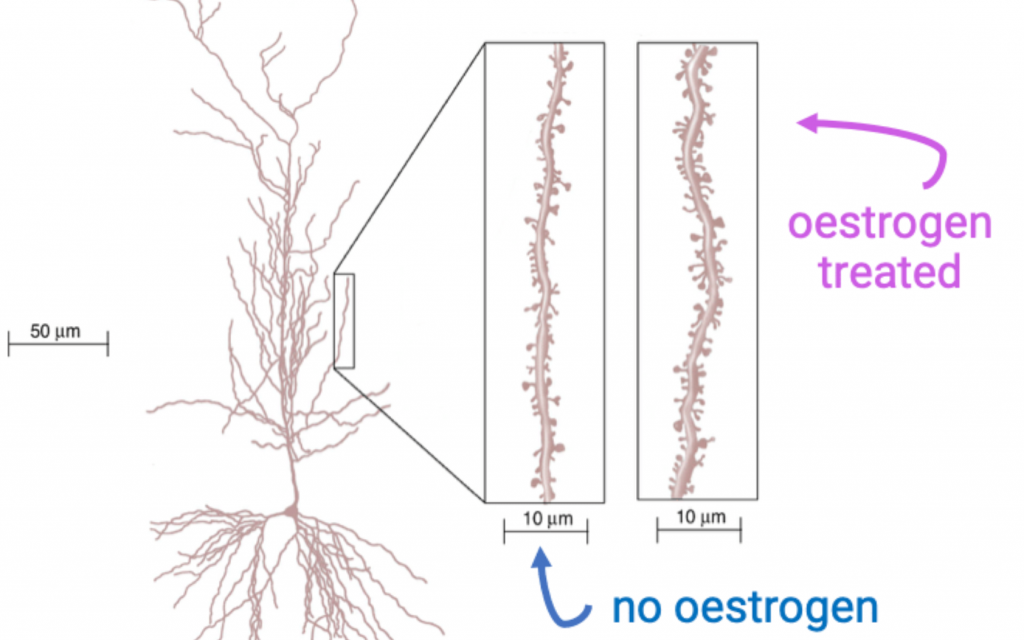
One of the most important and well-known effects of oestrogen is on the microstructure of neurons themselves, in particular the dendritic arbour of neurons.
Dendrites and spines (tiny buds on dendrites on which synapses form) sprout and retract over the course of oestrus cycle (the menstrual cycle equivalent in rodents) in response to the rise and fall of hormones.
Our brains are capable of plasticity and the dendritic spine is the major site of this activity. Spines in the hippocampus and cortex brain areas related to cognition (the fancy neuroscience term for thinking) and emotion regulation are highly sensitive to oestrogen fluctuations.
Normally, oestrogen directly modulates neurotransmitter systems, especially serotonin and dopamine. Oestrogen scales up neurotransmitter manufacture and release, blocks neurotransmitter re-uptake and degradation, regulates the growth and pruning of synapses, and modulates overall structural morphology of many brain regions.
Changes in oestrogen signalling (either through changes in oestrogen levels or changes in oestrogen receptors) will directly affect how these numerous brain circuits function, although the exact mechanisms by which menopause alters brain physiology to generate symptoms isn’t clear.
Oestrogen may impact glucose metabolism
One working hypothesis focuses on the metabolic link between oestrogen and healthy cell function.
Our brains metabolise 20% of our energy supplies, and the brain’s main fuel supply is glucose.
In women, oestrogen supports the biochemical pathways that use insulin and generate energy from glucose. So the menopausal drop in oestrogen may change how efficiently the brain uses glucose and in turn how well neurons function.
The link between oestrogen and glucose metabolism plays out most clearly in women who have their ovaries removed before they go through menopause (e.g. cancer treatment) — the abrupt drop in oestrogen levels is associated with an increased risk of developing Type II diabetes. The same increased risk for Type II diabetes is seen after natural menopause, whereas for women using HRT, glucose metabolism is typically normal.
I’ll save the wellbeing lifestyle lecture for another day, but the link between oestrogen, glucose metabolism and Type 2 diabetes highlights the importance of self-care and attention to exercise and healthy eating for women as they age.
In my next blog, I’ll be looking at one of the most common symptoms of menopause – the hot flash!
This is a long and detailed read. Click here to download the series as a PDF to read offline.
YOUR BRAIN ON MENOPAUSE: In this seven-part series I explore menopause from a brain health perspective with a particular focus on the neurobiology of hot flashes, sleep, mood and memory, the role of hormone therapies and their long-term effects on the brain. This is Part 2 and is based on excerpts from The Women’s Brain Book. The Neuroscience of Health, Hormones and Happiness.
Share the love
[Sassy_Social_Share]
8 Comments
Leave a Comment
About Dr Sarah
Neuroscientist, Author, Speaker, Director of The Neuroscience Academy suite of professional training programs.
Latest Posts
Free 10 day micro-training in neuroscience

Learn one neuroscience concept a day!
10 simple, bite-sized lessons in brain health, delivered daily to your inbox


Appropriate and appreciated topic menopause as a 53aged women, now no period for 5 months, unsure why so mentally and physically tired. Eating Mediterranean style diet, sleeping near 2 hours more. Senior generations never spoke about menopause. Thankyou Sarah for your work, regards Angela Davies.
Really appreciate learning more about the brain during menopause and the acknowledgement of how diverse our experience of menopause can be. Friends assured me their hot flashes lasted only about three years. 18 years since my last period and I still regularly have hot flashes!
FANTASTIC!
Please blog the next 5 as a matter of urgency!
🤣
Thank you!
I’m trying LOL!
Interesting. And to deal with it? What can we do to try to revet those effects?
Hold tight … more posts to come!
i like this article so much, it has a lot of info i need to know, thanks for sharing
Thanks for the educative write up, does the brain like contracts and retracts during flashes?thanks