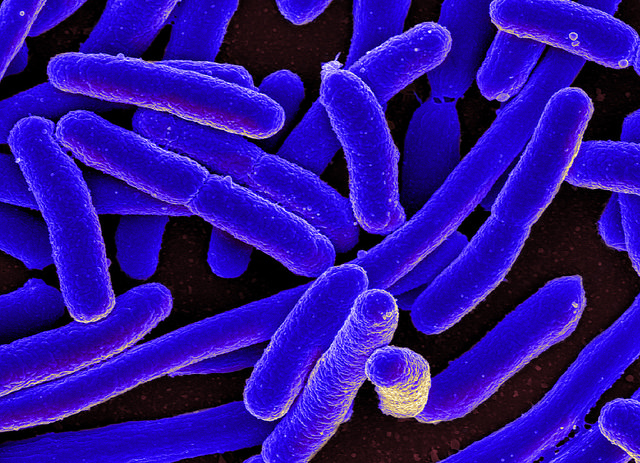
Coloured scanning electron micrograph of Escherichia coli, grown in culture (CC BY 2.0)
This is the first post in a series exploring the neurobiology of the gut-brain connection published in partnership with neuroscientist Dr Amy Reichelt.
Our brain and gut are intrinsically connected. We have ‘gut feelings’ about a person or event, and feel ‘butterflies’ in our stomach when something exciting happens. Neuroscientists have become increasingly aware that our gut may hold key insights into brain function.
The gut itself has what is often likened to a ‘mini-brain’ — an extensive network of neurons called the enteric nervous system. The brain and enteric nervous system talk, and the shared communication line between the two is often called the gut-brain axis.
The gut-brain superhighway
The gut communicates with the brain via hormones released into the bloodstream that cross the blood-brain barrier, controlling our desire for food. For example, the gut hormone ghrelin tells us when we’re hungry, and other hormones such as glucagon-like peptide 1 (GLP-1) influence satiety or tell us when we’re full. Such hormones act on the reward-signalling neural circuits in the brain, explaining why food tastes better when we are hungry.
The gut also makes neurotransmitters, which are the molecules neurons use to communicate at synapses. One such neurotransmitter is serotonin (aka 5-hydroxytryptamine, 5-HT). About 90% of the body’s total serotonin is made in the gut, the rest is made in the nervous system. In the gut, specialised enterochromaffin cells lining the wall of the gut make and secrete serotonin where it plays important role in controlling peristalsis — the wave-like contractions of the gut walls that squeeze food along the digestive tract. Some neurons in the enteric nervous system also make and use serotonin as a neurotransmitter.
Note! The gut is not the brain’s ‘serotonin factory’. Neurons in the brain make their own neurotransmitters. Also, gut-secreted serotonin (and other neurotransmitters) cannot cross the blood-brain-barrier, so it’s improbable gut serotonin directly influence brain function via the blood stream.
The brain-gut-microbiome axis
There is another important player in the gut-brain conversation. Our intestines are home to an entire ecosystem of microbes that control digestion, fight pathogens, and modulate hormone and neurotransmitter production. The collective of these microbes is termed the ‘gut microbiome’. An average person has about 1.5 kg of bacteria in their gut – similar to the weight of the brain! Gut bacteria also make the neurotransmitters including γ-aminobutyric acid (GABA), serotonin, dopamine and acetylcholine.
Gut bacteria talk to the enteric nervous system and the brain, but the precise method of communication is unknown — researchers call it ‘black box connectivity’. Possible lines of communication include via hormones, immune signalling molecules, metabolic pathways, and via the vagus nerve.
Squeaky clean mice
Much of the microbiome research to date has used germ-free mice raised in highly sterile conditions. Germ-free mice are born by Caesarean section, thereby preventing the transfer of microbes from their mother. They grow up inside sterile isolators, are fed purified food and water, and breathe filtered air. Germ-free mice offer a blank canvas when it comes to their gut microbiome.
Fecal microbiome transplants (FMTs aka poo transplants) into germ-free mice allow researchers to explore how a specific gut microbiome profile can change brain function. For example, after receiving a poo transplant, germ-free mice adopt the behavioural traits of the donor mouse. One study showed germ-free mice that received FMTs from stress-prone mice became more nervous in a new environment — essentially adopting nervousness from their poo-donor. In comparison, germ-free mice receiving FMTs from more curious and inquisitive mice became less anxious in strange situations.
These experiments suggest the presence and composition of gut microbiota provides a signal to the brain via the gut-brain axis that in turn modifies rodent emotions.
However, it’s very important to understand that germ-free mice are not typical mice. Germ-free mice are reared in artificial ‘bubble-like’ environments in the absence of micro-organisms to shape their immune systems. Their behaviour fundamentally differs from standard lab mice; particularly stress reactions and social responses.
Can we ‘balance’ the brain with bacteria?
Altering the microbiome through FMTs has potential to change brain chemistry. Case reports in humans suggest that FMTs may have therapeutic potential for disorders including autism, chronic fatigue syndrome and multiple sclerosis, but much more research is needed. There is a well-recognised ‘gap’ between rodent neuroscience research and application in humans.
In my next blog, I will discuss how scientists are manipulating the microbiome through the use of ‘psychobiotics’ to treat mood disorders and the use of probiotics and prebiotics as brain health supplements.
Dr Amy Reichelt is a neuroscientist with training in behaviour, psychology and molecular biology. She completed her PhD at Cardiff University in 2011 and went on to postdoctoral research fellowships at the University of Birmingham, UK and as an Australian Research Council Early Career Fellow at UNSW Sydney. She is currently a lecturer at RMIT University, Melbourne.
Her research examines what happens to the brain when it is exposed to environmental changes – such as junk food diets, exercise, stress, and drugs.
Amy is passionate about science communication and her career-defining 2016 TEDxSydney talk can be found here:
Amy is an avid Twitterer (find her @TheAmyR) and has written for The Conversation, The Guardian, and other news websites.
Her personal website is http://amyreichelt.com.
Share the love
[Sassy_Social_Share]
27 Comments
Leave a Comment
About Dr Sarah
Neuroscientist, Author, Speaker, Director of The Neuroscience Academy suite of professional training programs.
Latest Posts
Free 10 day micro-training in neuroscience

Learn one neuroscience concept a day!
10 simple, bite-sized lessons in brain health, delivered daily to your inbox


This is a very interesting overview. It is always challenging in an ever-emerging science to be able to know the difference between reality i.e. current facts – if there is such a thing in neuroscience – and the seeming leaps of speculation taken by the world of pseudo-science i.e. speculative connections.
Are you doing any work in the area of heart-brain connectivity or indeed heart-brain-gut connectivity as there seems to be a lot of opportunity for pseudo-science in this area.
The GPs and the medication they prescribed failed me – after I had been told because at my age I had the change (which had come and gone) and a side affect was the depressed state I was experiencing.
In fact it was my ICV (value in intestines) having a malfunctions (a post op traumer) and the more chemical drugs the main stream medico’s persisted I take the worse my depression got – years of this. I kept saying I felt poisoned and would have periods I would go cold turkey off all meds or may have taken my life. The was was that black and deep.
A NET CHIRO diagnosed the ICV problem and I kept away from chemical meds and spent a year on mashed green and over cooked beef, I was in such a bad state, and now I am starting to get back to a more normal diet with an ICV behaving nearly normally and MOST OF ALL my head is feeling very good and I am
In control of it, to a point where I have started to study in the field of Gut Mind Body holistic therapies.
Looking so forward to this study week! Fascinating information, especially for Healers!
It’s great to be able to read science backed, hype-free facts on this topic, in a simple to understand text from 2 non-biased neuroscientists! Looking forward to the next 5 installments!!
It’s our pleasure!
Thanks Sarah, very interesting article. Just wondering if in the future FMT’s may be used to treat people with depression or anxiety and your thoughts on that?
That’ll be addressed in a future blog … watch this space!
Excellent Part ! article…I find this topic fascinating..and also really enjoy Dr. Amy’s TEDx talk…looking forward to learning more about probiotics and prebiotics and how they do or might affect brain function…
I am interested to learn more about psychobiotics- this is new to me. So much to digest in the field in gut-brain connection.
Very informative and keen to learn more Sarah ~ thank you
Can we please please please stop saying that we have another brain in our gut!
I hear what you’re saying, and completely agree we don’t have a brain in our gut. Therefore the exact phrase ‘mini brain’ was in placed in inverted commas.
I’m not a brain scientist, or anything close, just an interested party. I wonder whether diseases of the digestive system, such as Crohn’s disease (which I have, along with other auto immune conditions) affect the brain gut connection? And if so, in what way?
Sarah – thanks so much for taking the time to cover this topic. I have read hundreds of articles over the past 3 years in an effort to gain a greater understanding of our “gut brain” – your ability to dig into the research and communicate the information in a simple and straightforward ( no-nonsense ) way is a gift. Thank you.
My Papillon was diagnosed by the vet as having IBS. His response to Boarding Kennels. As a Dog Behaviourist I’ve taught him alternate behaviours to cope with stressful situations. As he has learned new skills his anxieties have abated and so has his acute separation anxiety. Last stint in the boarding kennels realised a dog with NO diarrhoea staining his profuse white hind furnishings.
Wonderful that work is being done in this field, thank you for freely publishing it. (Sideline). I am 90 years old ,always taken for much younger, very much fitter than than i was before commemcing eating a diet of fresh quality foods 45 years ago.
Knowing that the brain extends, via neurons, to every part of the body, including the gut I would certainly like to hear more about the connection and interactions etc..
Hi Paula,
Diseases and disorders that increase inflammation in the body, such as Crohn’s disease are indeed linked to changes in the brain. As a neuroscientist I am very interested in how peripheral inflammatory responses are transmitted to the brain, and the effects this has on brain function.
I’m personally very interested in this as I’ve had FMT therapy. I have Ankolysing Spondyaloarthritis and Psoriatic Arthritis, and had associated Lymphocytic Colitis – the latter was the specific target for the FMT therapy. It worked, the Lymphocytic Colitis disappeared…
I didn;t notice any change in state other than that – but then I wasn’t looking for behaviour change…
I could put you in touch with the professor who did my FMT therapy if you’reinterested? I’m thinking he would 1. have a bank of information and 2. might be interested in doing some correlated research around this…
Excellent article from a neuroscience perspective with clear concise explanations
So much knowledge in this article. What a fascinating study on FMT and the impact they have in comparison to the germ-free mice. The microbiome is truly such a mysterious and revolutionary topic.