Does CBT Teach Your Prefrontal Cortex To Keep Emotions In Check?
In 2014, science journalist Emily Anthes wrote a piece on cognitive behavioural therapy (CBT). Here are a few of the highlights from Anthes’ piece (and 2023 research updates 🌱.)
Cognitive behavioural therapy (CBT) lifts depression 🌱
CBT aims to help people to identify and change negative, self-destructive thought patterns. The programme equipped patients with the skills they needed to critically examine their negative beliefs and become their own therapists.
It doesn’t work for everyone, but the stats on recovery showed an interesting story when compared to pharmacotherapy:
- 42–66% of patients no longer meet the criteria for depression after CBT.
- 22–40% of patients emerge from depression with drugs alone.
What are the ‘active ingredients’ of CBT?
CBT ‘works’ (for 42-66% of depressed people), but no one knows the ‘active ingredients’. Changed thought patterns? Positive thinking? The bond with the therapist? 🌱
Does the therapy relieve depression by changing someone’s thought patterns, or is the new pattern of positive thinking a consequence of someone’s improved mental health?
Research into the CBT mechanism
To begin to unravel the mechanisms, researchers studied recordings of CBT sessions.
“…what you want to do is get inside the moment or moments when someone has a positive therapeutic change and try to understand what’s shifting in just those moments.”
Research has revealed any depressed adults undergoing CBT experienced ‘sudden gains’, in which their symptoms lessened significantly between two therapeutic sessions. These rapid changes accounted for more than half of the patients’ total improvement over the course of treatment. Indeed altering a person’s thinking style may indeed lead to recovery. 🌟
Researchers have also shown that learning mental coping skills may be the most critical kind of cognitive change during CBT.
“The cardinal skill is catching your thoughts in a moment where your mood takes a turn for the worse and thinking through the accuracy of your thoughts at that moment.”
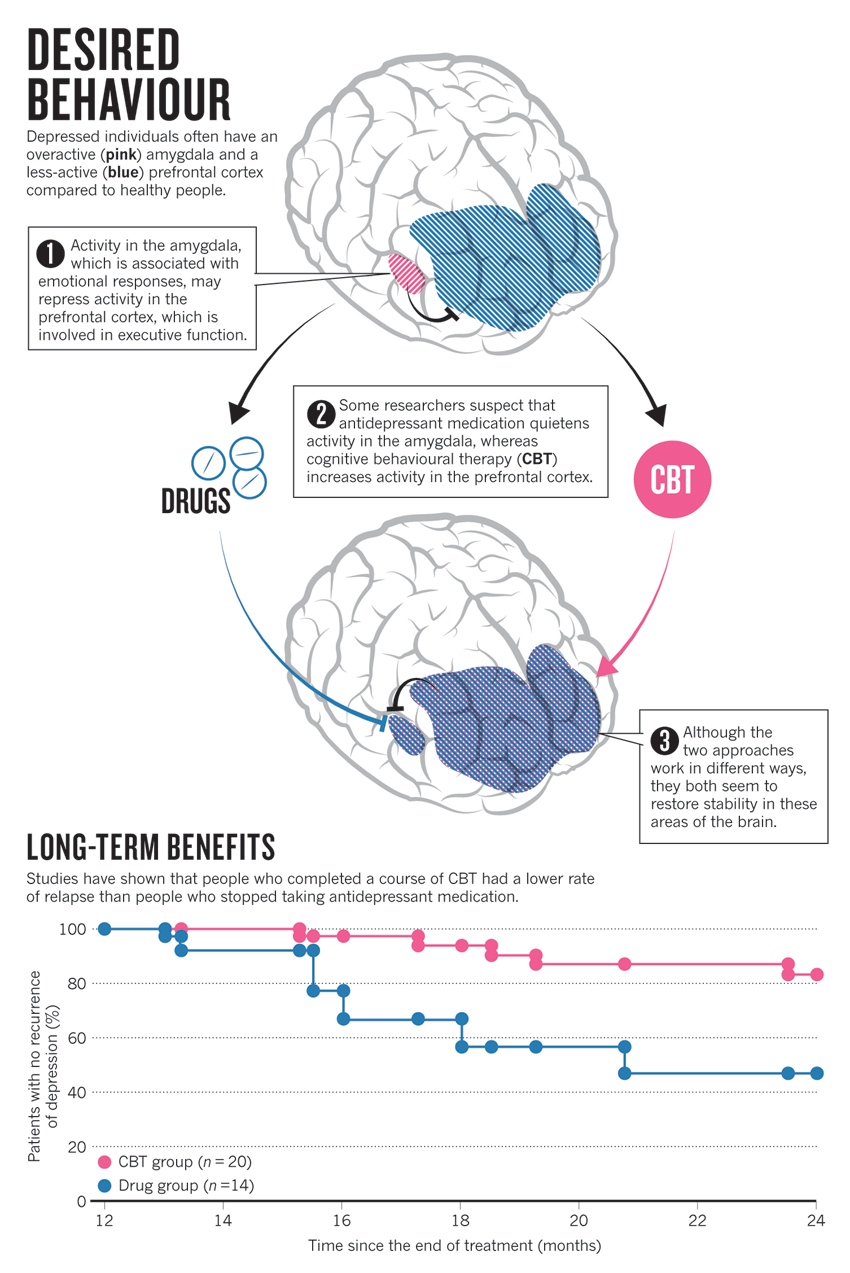
Brain imaging studies have focussed on two brain areas—the prefrontal cortex, responsible for complex mental tasks such as self-control and planning, and the limbic system — including the amygdala — which is involved in emotional processing.
In healthy people, the prefrontal cortex can inhibit amygdala activity, keeping emotions in check. But imaging shows that in many people with depression, the prefrontal cortex seems to be less active.
“Depressed people have what you might think of as a trigger-happy amygdala.”
One study showed that depressed adults had increased activity levels in the amygdala when performing an emotional task and reduced activity levels in the dorsolateral prefrontal cortex when performing a cognitive task. CBT reversed this situation.
Researchers speculate that CBT — focusing on controlling thoughts — re-engages the underactive prefrontal cortex, which, in turn, helps to quieten the hyperactive limbic system. 🌟
“Cognitive therapy teaches you to step in and use your prefrontal cortex rather than letting your emotions run away.”
New 🌱and important 🌟 2023 Research Updates:
🌟 The impact of CBT for depression is modest to large, and it persists for at least a year after therapy has ended.
A 2023 meta-analysis of 409 trials (including 52,702 people, 27,000 of whom received CBT) found CBT for depression is effective (CBT performs better than control conditions for reducing depression symptoms up to 12 months later for many people in different situations).
However, CBT was not superior to over other psychotherapies for depression. The research also concluded CBT appears to be as effective as pharmacotherapies in the short term but more effective in the longer term.
🌟 People who experience a ‘sudden gain’ during their CBT sessions tend to have better longer-term outcomes following treatment.
However, these changes tend to have a more significant effect on recovery for those with depression or anxiety when compared to those receiving CBT for other mental health conditions. The number of CBT sessions can also diminish the improvements following a ‘sudden gains’ experience.
Interestingly, depression severity doesn’t influence the ‘sudden gains’. Instead, individuals with considerable variability in their symptoms are more likely to experience sudden gains. This suggests cognitive flexibility could be a key contributor to this CBT phenomenon.
🌟 New brain imaging research has revealed that CBT strengthens the neural connections between the prefrontal cortex and the amygdala.
The improved connectivity between these two brain regions following CBT likely reflects enhanced top-down control of mood and emotions. CBT can reduce the activity of the amygdala (and other limbic structures), which predicts improvements in symptoms of depression and anxiety.
On the other hand, studies have observed reductions in connectivity between the prefrontal cortex and the anterior cingulate cortex following CBT. This network is involved in negative self-perception and ruminating thoughts in patients with depression. The weaker the connectivity of this pathway after CBT, the greater the improvements in depressive symptoms.
🌱 People with mild to moderate depression may respond better to CBT than those with severe depression.
However, those with severe depression can still benefit from CBT. Instead, when depressive symptoms become more severe, the patient may require a more comprehensive treatment plan. Research indicates that combining CBT with anti-depressants and controlling for other factors, such as therapists’ experience, can deliver the greatest effect for people with severe depression.
🌱 Patient-therapist bond improves depressive symptoms.
Though the therapeutic bond can affect outcomes at all stages of therapy, it appears to have the strongest influence during the later stages of CBT. However, it’s unclear whether improvements in symptoms cause feelings of increased bonding or if the bond itself improves symptoms.
Share the love
[Sassy_Social_Share]
3 Comments
Leave a Comment
About Dr Sarah
Neuroscientist, Author, Speaker, Director of The Neuroscience Academy suite of professional training programs.
Latest Posts
Free 10 day micro-training in neuroscience

Learn one neuroscience concept a day!
10 simple, bite-sized lessons in brain health, delivered daily to your inbox


This in a comment in an email today …
Hi Dr McKay,
Thank you for your really interesting communications. I’m a 57 year old hospital social worker (for about 16 years) and I’m fascinated by the emerging area of neuroscience. In my own practice I undertook a CBT (REBT) course which profoundly changed my life and made my challenges much more bearable I think I was extremely fortunate as there were two presenters on the course but only one was a really gifted teacher. I found the course very confronting at times and truly in the beginning if I could have pulled out I would have! But like a lot of difficult situations there were great rewards in completing the course.
For me it was the consistency of the therapy with the ABC technique plus the teaching of unconditional self acceptance which I think many of us completely miss. It’s quite different from ‘self-esteem’ as we tend to refer to an internal belief of value and confidence. And not “positive thinking” at all – rather rational thinking via a series of disputing techniques. It’s incredible to watch a skilled therapist teach a depressed (or anxious) person how to think differently about how they see the situation. And understand the underlying often dysfunctional beliefs that we all learn.
Best Wishes
Jane MacArthur (who said she was happy for this comment to be share 🙂
I am a retired English language teacher for adult migrants – now involved in a range of voluntary work: helping translate texts into English, SRE (Special Religious Education) once a week with Year 2 children, a 1:1 arrangement for teaching Tai Chi and some advocacy.
My personal experience with CBT combined with medication was quite brilliant, thanks to the psychiatrist who worked with me for 11 years (1993 – 2005) and bulk billed the entire treatment. My amygdala had been previously been so hyperactive that at one point an acupuncture treatment normally used to sedate elephants just barely calmed me down.
Dr Quinn, the psychiatrist who helped me so much, died last year. I am sure that his professional training in CBT, combined with an excellent knowledge of the effects of medications and brilliant intuition, has kept me out of trouble from both hypomanic and depressive episodes for the last 16 years. I had two hypomanic episodes prior to seeing Dr Quinn – one in January 1991 and one in January 1996. I had never experienced anything like these episodes before, though I believe I had several undiagnosed depressive episodes in my 20s. Dr Quinn diagnosed severe PTSD and Bipolar Disorder II (bipolar disorder triggered by traumatic memories).
I experienced these memories primarily emotionally and mentally, sometimes physically, as body memories, and on two rare occasions, which I found the most devastating, as brief visual vignettes which included with emotion, mental awareness and the sense of touch.
On reading this article it is clear to me that Dr Quinn gave me the best possible treatment by being able to combine CBT with medication. In addition, I have been married for over 30 years and my husband has been incredibly supportive at all times.
I am willing to share this response to your article. I look forward to learning more!
This is common sense I feel. Or maybe I have been very lucky to have a small group of very close friends where I feel comfortable to discuss my life warts and all. Family ties are also very important to stability and well being. Actually probably in my opinion the most important.
I have had what I consider bouts of depression over the years, a bad relationship, death in the family and a family member who was in trouble with police. I coped on a daily basis because I managed to switch off my negative thoughts when I was at work. This ability helped me through. No one I worked with knew what I was going through.
On the whole I realise my problems are nothing compared to others and I certainly have not had any traumatic issues to deal with.